|
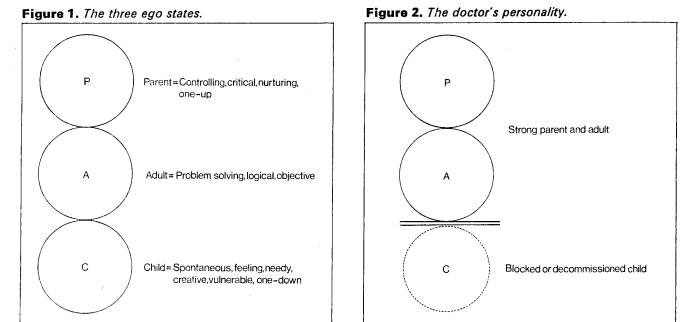
David Zigmond Those who care for others often have great difficulty in caring for themselves. Doctors are notoriously bad patients. Those who must care for them are often confused by the perplexing tangle of feelings which may accompany looking after a sick colleague. In the last two decades there have been some interesting though ominous studies on the morbidity and troubles of doctors. Perhaps the most striking data concern suicide statistics. All the studies concur in demonstrating a rate of suicide among doctors that is at least double that of the rest of the population (Rose and Rosow 1973; J. Amer. Med. Ass. 1974). It is significantly higher than comparable economic and 'non-helping' professional classes. The highest rate is found among psychiatrists, followed by physicians, surgeons and finally paediatricians (Blachey et al. 1968). In concurrence with suicide, the rate of marital breakdown and drug abuse among doctors is similarly high (a'Brook et al. 1963; Emshwiller 1973; Hospital Physcn. 1970; Vaillant et al. 1970; Vincent et al. 1969). Quite as important, though not as accessible to measurement, is the tragedy of 'marital rot'. By this I mean the marriage that has lost its meaning in terms of emotional closeness, intimacy and enriched sharing; this may be the commonest, though least spectacular, of doctors' problems in living (Lewis 1965). Other studies are equally illuminating in completing the pattern. Doctors are less likely to become psychotic or act-out in ways that are socially dissonant or compromising (Duffy 1967; Duffy and Litin 1964). They are less likely to be convicted of crimes of violence, burglary and causing an affray. Alcoholism among doctors is similarly concealed (Vaillant et al. 1972); it is likely that the problems will be borne by his colleagues and family, but the wider community will be left in peace. What the Statistics Mean It may be inferred from the foregoing data that doctors, together with others in the caring professions, are incapable of acknowledging or allowing themselves the frailties they may look after so assiduously in others. When it comes to a crisis in our own lives it seems that there are many doctors who would rather be seen dead than in any way compromised, dependent or weak. Our armour of apparent omniscience and omnipotence has taken years to develop and is hard to discard. Many of us have developed a compulsive persona of exemplary independence, strength and integrity which we relinquish only under the greatest duress; regression is for patients, not doctors. The structure and nature of many medical transactions and rituals conserve the position of the doctor's executive and emotional power. The medical model itself may have such a conservative function. I have examined this problem in an earlier article, and will do so in a future article (Zigmond 1976 and 1977). It is not only as individuals that we suffer and perpetuate this dilemma; we collude together to minimize, conceal or deny these problems. The ethos of the stiff upper lip and coping-at-all-costs is learned early in our training, is ubiquitous and is played extremely hard, particularly in hospitals. How many of us would allow ourselves to be openly depressed and comforted by a colleague? We are much more likely to maintain a stoical and inscrutable front and urge others to do likewise—unless they are patients, of course. From my own emotional experiences and from what other doctors have told me, I can only deduce that there is a tacit but severe conspiracy of silence regarding this painful area. The lack of emotional rapport and support within the caring professions is paradoxical but gross. Our expectations of ourselves and others to remain strong and intact whatever the conditions are unyielding. We allow default from this only in heavily ritualized, contained and secretive settings. If a doctor is a psychiatrist, for example, it may be accepted that he will seek psychotherapy as 'part of his training'. However, in many ways what he is doing is stealing away to a special place where, in total privacy, he has someone to listen to and accept the more vulnerable and dependent parts of himself. He is paying someone to respond to him as a feeling human being. It is remarkable and ironic that other groups who claim much less expertise and concern about human suffering cope with it so much better in members of their own group. The emotional support, accommodation and latitude that people allow one another in shops, industrial organizations and so forth frequently outstrips our equivalent performance and attitudes within the caring professions. The following account illustrates the potentially tragic nature of such collusive and defensive responses. The Case of Dr X Dr X was a junior hospital psychiatrist who started his first post in this specialty at the same time as I. He had just arrived in the UK from the Middle East, had no family or friends in this country and resided in the hospital. He had studied medicine later than usual and was in his mid- thirties, despite his junior rank. His manner at work had always been appeasing, over-conscientious and highly introvert He was an extremely lonely man who seemed to spend his off-duty hours either studying or impassively watching television. Slowly his behaviour became increasingly capricious, prickly and withdrawn. Nursing staff observed him behaving oddly and irascibly with patients. On one occasion he sprinkled a patient with water while chanting verses from the Koran, explaining that the patient's 'being would be made pure'. Soon after this he wrote a long, untrue and defamatory account about another doctor in a patient's case notes. Largely to satisfy the nursing staff's insecurity it was decided that Dr X's clinical responsibility should be undertaken by another doctor. However, Dr X was not confronted with this and still held tenure of his post. It was hoped that such 'papering over the cracks' would save face for Dr X, that he would not be compromised, that no one would feel awkward and that the psychiatric unit would somehow continue to muddle along. At this point I asked to see Dr Y, the senior consultant in the hospital. I realized I was a novice but felt perturbed by what I saw. I felt that the situation was confusing and jeopardizing patient-care, and that Dr X was extremely depressed and paranoid. I expressed the belief that Dr X was being treated with duplicity, and that this fed into his sense of mistrust, powerlessness and alienation. It would be far better, I maintained, to acknowledge openly his serious problems, to relieve him of his work and to find him help outside the hospital. Dr Y's response was defensive, authoritarian and dismissive. I was made to feel that such a breach of the conspiracy of silence was inapt, impudent and unethical. Dr X later died from a suicidal overdose while still employed at the hospital. It is doubtful that this man would have died amidst these circumstances in any other but a `caring' profession. He would have received help. Doctors' Dilemmas Doctors in clinical practice have decisions and dilemmas which may be inescapable, and which contain some of the most private and powerful material which occurs in human transactions. Consider the following situations that many of us may have become seasoned to, though hopefully not thoughtless about: Mr A. has a malignant neoplasm and he does not know. What should I say? … Shall I tell him? … or if not he, his wife? Mrs B.'s condition warrants my exploring her vagina and rectum. Mr D. has had ulcerative colitis for 10 years. I think he should now have his colon removed and be left with a lifelong ileostomy. I will not resuscitate Mr E. The prospective quality of his future existence seems unworthwhile to me. I do not understand Miss F.'s frigidity. Perhaps I shall ask her about her masturbatory fantasies. Although Mrs G. denies being ill, does not wish to consider therapy and has committed no crime, I consider her behaviour to be deviant. I will have her taken to an institution and treated against her will. All of these experiences are dramatic or devastating for the patient. It is sobering to consider how common these situations may become for us. These are crucial and decisive scenes for our patients, and the doctors' tools are correspondingly powerful and dangerous. In consequence can only use them legitimately if we are: strong, patient, worldly, sagacious, unselfish, responsible, infinitely knowledgeable, highly ethical and scrupulous, uncorrupted by power, aggression, sexuality and greed, and always intact and alert to the most demanding and diverse situations. In the face of such demands we cannot be: demanding for ourselves when others need us, unable to face what is there, uncomprehending, self-indulgent, indecisive, ignorant and weak. A Note on Transactional Analysis Transactional analysis is a highly sophisticated though clear account and explanation of human development, interaction and dysfunction. For this article I am using only some simplified rudiments of the theory. Transactional analysis postulates that we all have three Ego-States and that usually we are operating in only one of these at any one time. An Ego-State is a system of feeling, thinking and behaviour, all of which are inter-linked. The three Ego-States are called Parent, Adult and Child. Parent and Child ego-states are generally largely formed by the time we are eight years of age. The Parent develops from what we are taught by actual parents and other influential adults. It derives not only from what we are told explicitly but also what we observe parent figures doing. The Parent is thus the seat of nurturing and controlling impulses and behaviour, whether to ourselves or others. Subjectively our Parent feels protective or critical, and has the conviction of knowing what is correct and ethical even if this is not, in fact, the case. Generally when we are in our Parent, we feel secure and relate from a one-up position of 'right' and strength. The Child, reciprocally, is the world of experiences that we felt as real children and still feel now. It has all the qualities of the natural child as well as the child that has learned to adapt to survive amidst more powerful adults. The Natural Child is fun-loving, pleasure-seeking, emotionally demanding and labile, creative, curious, impulsive, unashamed, greedy and loving. This bit of us believes in magic and may feel either omnipotent or completely helpless, just as we all did as small children. It is the part of us that shares and experiences with vividness and immediacy. As children, however, we also had to learn the strategies of living with those whom we were dependent upon, and these dependent patterns of compliant or rebellious behaviour make up the Adapted Child. The Adult is the reality principle in the personality. It is capable of observing, assessing, storing and patterning information in an objective way. It can turn these logical powers externally to the outside world, or internally to monitor and mediate between the other two ego-states. In many ways the Adult may be seen to function like a computer. For simplicity we can represent these personality functions diagrammatically (Figure 1).
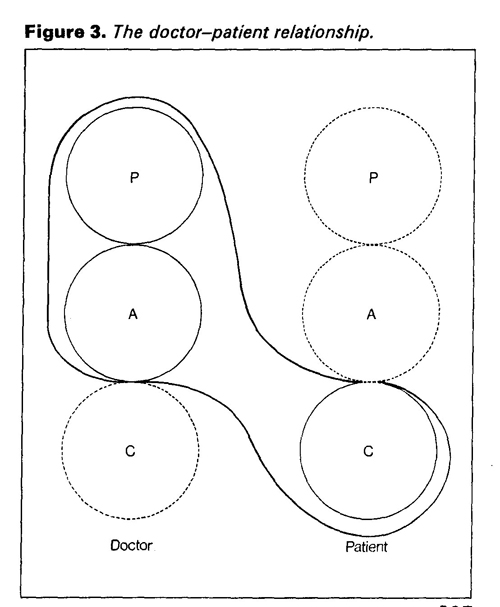
Doctors' Personality Structure In the preceding sections I have outlined how people in the caring professions tend to take better care of others' needs than they do of their own. Because of both our working dilemmas and our personality structure, we tend to function largely in our Parent and Adult. We may thrive on looking after seriously sick or compromised people, and we may consider ourselves expert in knowing what is good for others. Many of us pride ourselves on our accurate observation, fund of factual knowledge, and problem-solving ability. What we are often out of touch with is our Child. The world of chaos, strong-feelings, spontaneity and vulnerability is kept strongly in check, if not denied, by our Parent and Adult ego systems. A modified diagram of our personality can be represented as shown in Figure 2. Symbiosis When we deny powerful needs and impulses in ourselves, we will be either intolerant or solicitous of these attributes in others. If the latter, then it is very likely we will work in one of the caring professions. In effect we seek out and look after the part in other people that we disown or suppress in ourselves. Our needs may then be fulfilled vicariously through a state of mutual dependence. Such an interlocked relationship may be diagrammed as in Figure 3. Figure 3. The doctor—patient relationship
The doctor's part in such a tacit contract reads: "I will be strong if you will be weak. I will support, protect and guide you so long as you are helpless and obedient. I will not express my feelings so you must have and enact them for me". Reciprocally the patient's role in this collusion reads : "If you will be my Grown-up then I will make you feel clever, potent and important. To make sure that's so I will be passive, aimless and dependent". Such dependence upon our patients for our sense of power and vicarious expression of locked-up feeling is often not conscious. In the short term this may be harmless. The long-term effects, however, may be similar to many other relationships which can only thrive on a radically unequal power distribution. Because gratification of both partners depends on a rigid status-quo where no growth is possible, a sense of entrapment, waste and resentment is likely to evolve. This may account for many harried and depressed doctors who are uncomprehendingly dependent on their patients' dependence. The Making and Breaking of Doctors The factors that motivate us to become doctors are often those that lead to the emotional problems that I have described. It is for this reason that I wish to discuss briefly and generally the kind of family and social backgrounds that contribute to the formation of our particular personality structure. Most doctors come from middle-class or upper-class backgrounds which are likely to have a strong parental ethic. There is a tendency in this section of society to pride itself on knowing best what is good for other members of society. It is not only doctors, of course, who emerge from this patriarchal mould; we also produce lawyers, captains of industry, clergymen and legislators. We are prepared early for these tasks. How many of us can still remember being told prematurely to 'grow up', `don't be silly' or 'do be more responsible' when we were not yet eight years old and childhood with all its tumult should have been our right? Later, this precocious acceleration into adulthood and responsibility may have been compounded even further by education in Public Schools. I myself remember at 11 years of age standing alone with my tuck-box on the station platform, fighting back the fear and tears and trying bravely to look grown up. It was many years before I successfully excavated and paid attention to my buried Child ego system. There may also be more particular family factors that contribute to this problem. Often we come from subtly deprived backgrounds, where we learn that it is not profitable for us to make demands, show our feelings or be weak, though we may consider it permissible in others. Perhaps as children our emotional life was felt not to count, and it was only our performance and behaviour that were recognized. From such conditioning we are liable not to value ourselves for what we are or how we feel, but only what we do. Such a central sense of dissatisfaction with ourselves may account for much of our motivation in seeking out the compromised parts of others. It may be that in so doing we find some kind of symbolic union and allay our own loneliness and sense of incompleteness. What Can be Done? It may be said that all activity has its psychopathology, and thus its sheer ubiquity should make it acceptable. Secretive and shamed conspiracies of silence about these subjects only add to inapt feelings of guilt and inadequacy. Many of us become silently burdened and depressed because of the way we are doomed to fall short of the perfectionist standards we set ourselves in collusion with our colleagues. Such training in being everybody else's exemplary grown-up starts early and should be countered early. Many of the formative factors have complex social and political roots, and it is unlikely that these could be changed rapidly. However, these problems could be openly and compassionately broached and discussed from the earliest years of medical training. Balint Groups for general practitioners have shown the widespread need for such forum and comradeship, but this approach evidently should be instituted earlier. The competent and sensitive doctor need not run the risk of being racked with paternalism, or self-doubt and self- recrimination. Neither need he be dependent on his patients to help them. References Brook, M. F., Hailstone, J. D. and McLaughlin, E. J., Brit. Med. J., 1963, 113, 1013. Blachey, P. F., Disher, W. and Roduner, G., Bull. Suic., 1 December, 1968. Duffy, J. C. and Litin, E. M., J. Amer. Med. Ass., 1964, 189, 989. Duffy, J. C., Wed. Tribune, 1967, 8, 15. Emshwiller, Med. Times, 1973, 101, 58. Hosp. Phycn., 1970, 6, 60. J. Amer. Mei. Ass., 1974, 228, 1149. Lewis, J. M., Texas State J. Med., 1965, 61, 615. Rose, K. D. and Rosow, C., Arch. Gen. Psych., 1973, 29, 800. Vaillant, G. E., Brighton, J. R. and MacArthur, C., New Engl. J Med., 1970, 282, 365. Vaillant, G. F., Brighton, J. R. and MacArthur, C., New Engl. J Med., 1972, 287, 372. Vincent, M. O., Robinson, E. A. and Latt, L., Canad. Med. Ass. J., 1969, 100, 403. Zigmond, D., Hospital Update, 1976, 2, 424. Zigmond, C., 'Scientific psychiatry—progress or regress?' Update, 1977, in press. David Zigmond, MB, CH.B, DPM, MRCGP, is Senior Registrar in the Departure of Psychological Medicine at University College Hospital, London. He is also a member of the Institute of Transactional Analysis. JUNE 1977/HOSPITAL UPDATE 325:329 Special Article Contents Copyright ©; Dr David Zigmond 2007 Interested? Many articles exploring similar themes are available via David Zigmond’s home page on www.marco-learningsystems.com David Zigmond would be pleased to receive your FEEDBACK
|