|
Three Types of Encounter
in the Healing Arts: DAVID ZIGMOND, MB ChB
MRCGP DPM Summary: Western Medical and Psychiatric practice, anchored to its theoretical base of scientific determinism, tends to interventions that are administrative and prescriptive. This is derived from, and reflected in, the way in which knowledge is constructed, and the use of language. While this pattern of practice often works well in acute, circumscribed physical syndromes, it is usually far less effective when dealing with other, more frequently encountered, patterns of distress. In such situations the doctor needs to develop alternative ways of meeting and understanding his patient, which implies change in the 'metabolism' of language and knowledge. The discipline and discrimination involved in orchestrating these various kinds of encounter may give us a fresh perspective of 'holism'. A clinical case is described and a model presented to illustrate and amplify these principles. _____________________________________________________________
William Hazlitt On People of Sense, 1826
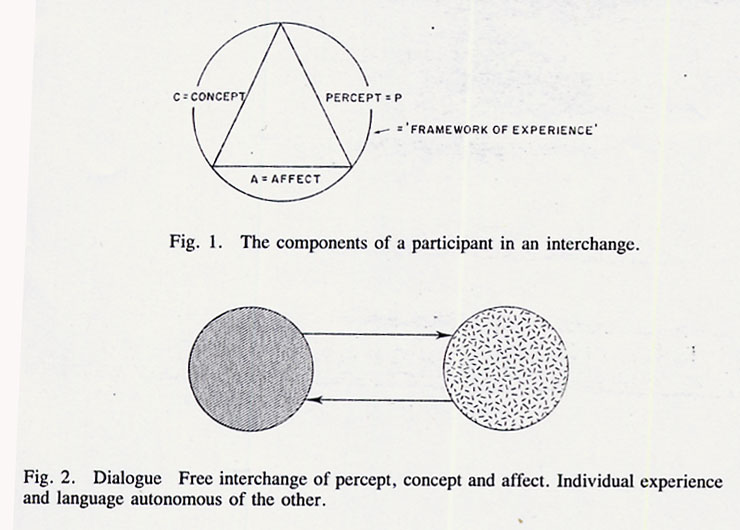
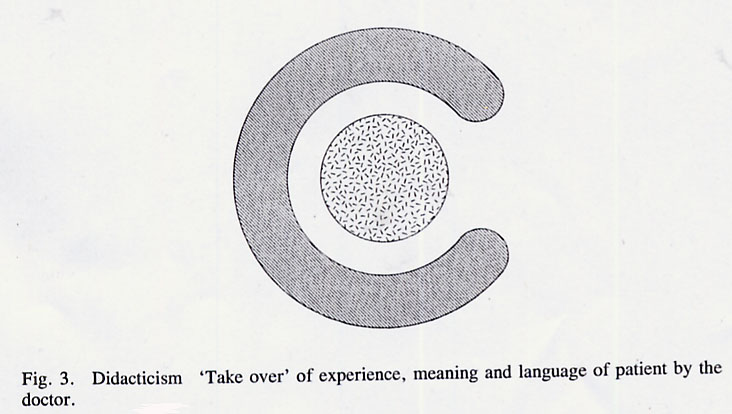
Thomas Szasz The Second Sin, 1973 Distress foreshadows and reflects fear and uncertainty in us all, and with it, to greater or lesser extent, the wish for the potent and protective figure or formula that will illuminate our way and absolve us the burdens of confusion, pain and the unknown. In our largest social groups we enact this in our investment in our choice (or extinction of choice) of political leadership, or legal and religious institutions. On our own, or in our most intimate groups, we devise more personal and idiosyncratic beliefs, rituals and protocols to ward off the potential storms or deserts of uncertainty. Medicine and the healing arts span both these realms. At the public level, the doctor's white coat, his portentous professional institutions, and quasi-militaristic career structure all serve, in large part, to convey a variety of images, notions and experiences that create a sense of authority, confidence and safety. At a more private level, the doctor's use of technical language, and the way in which he makes physical contact with a patient, have the same psychological and social aims of ritualizing control, management and predictability. Such behaviours work best when they are harnessed to visible and effective problem-solving, such as an acute surgical emergency, but the further we depart from this type of situation, the more problematic this style of approach may become. There are many kinds of distress which come to many kinds of healers where this type of structured and prescriptive manner becomes, at best, cumbersome, ineffective and insensitive, or at worst, infantilizing, insulting, injurious, and even corrupt by way of engendering unwarranted helplessness or damage in the recipient. It is, perhaps, the doctor's most challenging and unending task of self- education to discriminate when, how and to what degree to structure, define and manage what a patient brings to him in order to confer authority and predictability on the situation, and when, rather, to abandon such predication so that new forms of knowledge and interchange may evolve, which themselves spawn their own kinds of diagnosis and healing. To understand more fully the roots and ramifications of these issues, we need to look at how we build up 'knowledge' and how this is transmitted or changed by the use of language. Both of these 'elements' — cognition and linguistics — are mechanisms underlying the more observable 'compounds' of patterns of practice that will be considered. For this reason a brief theoretical diversion is offered here to underpin considerations of language and knowledge that run as developing themes through this paper. It will be seen that such apparently 'academic' notions have an important, even determining, relationship to the important issues of dependency, autonomy, responsibility and awareness that many regard as crucial factors in healing and the maintenance of health. Dialogue: the preliminary encounter When any two individuals come together to relate and to communicate, each has his own 'framework of experience'. This comprises awareness of himself and the external world (percept); his ideas, theories or expectations concerning himself and the world (concept); and a feeling state accompanying these two (affect). Figure 1 illustrates this as a coherent system, the circle encompassing the triangle denotes the individual's framework of experience at the time of the interchange, expressed verbally in this kind of encounter in 'individual language', where each participant's utterances remain relatively uninfluenced by the other, and thus idiosyncratic. In a 'dialogue', then, there is a free interchange of these components of experience, so that each will bring to the encounter elements of all three in his own manner, as a kind of exchange. Importantly, in the realm of dialogue, the experience and language of each participant remains autonomous of the other so that a 'free-trade' situation operates, as indicated in Figure 2. Note, also, that there is a distance between the two, which buffers each individual from any unwanted 'trespass', invasion or inclusion by the other.
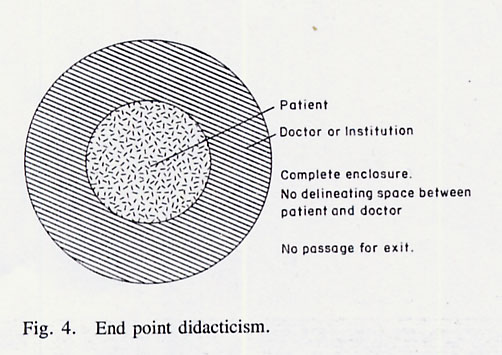
There are, evidently, innumerable everyday examples of dialogue where individuals make contact in a manner that retains, intact and separate, the framework of experience of each participant. Let us look at how this operates in a typical and authentic medical situation. Situation 1: Mrs G., a recently widowed woman of 60, consulted her doctor, Dr H., about pains in her chest, particularly on awakening in the small hours of the morning, when she would become frightened by the unknown-ness of her distress and her alone-ness in having to endure it. She described her mixture of physical sensations (percept), the limited sense she made of them (concept) and the feelings which accompanied them (affect), while Dr H. attempted to structure what she communicated to him and what he observed (P) by referring these to both the organizing concepts he had learned in his medical training (C) and, rather less, the feeling that arose in him during the consultation (A). He elaborated this process by asking her some routine questions about her chest pains and emotional state, and performing a physical examination. In attempting to fit all this 'information' about Mrs G. into his professionally learned organizing concepts (diagnoses), the doctor became aware of his difficulty in this regard; he was most concerned about her heart, although some features were not typical of this source. The other categories that came to his mind focused instead on Mrs G.'s oesophagus or mind; in regard to the latter she had described to him her fear, and she appeared rather sad and tense. Dr H. shared the dilemma arising from their dialogue, by saying 'Well I'm not sure what's wrong with you, Mrs G., I can't find anything on examination, but I think you should have some tests done at the hospital to see if there's any problem that I can't detect here, but which may need attention. I'll ask Dr J. to see you.’ Let us stand back from this situation and see what has emerged. Mrs G. and her doctor are in a 'free-trade' situation where they exchange unorganized 'bits' of experience, feeling or conceptualization, each with a different emphasis. The patient's main concerns and communications are of her disturbed bodily sensations (P), and emotional state (A); her ideas about these (C) are primitive and poorly organised. The doctor's focus is an attempt to form an organizing diagnosis (C), from what he observed and hears (P); Dr H. did not pay much attention to the feeling of protectiveness and sadness (A) aroused in him by Mrs G.'s presence, he was too busy attempting to subsume Mrs G.'s story and their encounter to a well-defined form of his own thought and language (a medical diagnosis) which would transform the 'dialogue' into a form of 'didacticism', a form of interchange to be considered presently. His failure to do so urged him to refer the unfinished dialogue to Dr J., who, he hoped, would complete the transformation. Didacticism: the organizing encounter Situation 2: When Mrs G. went for her appointment with Dr J,. she was aware that she was going to a 'specialist'; someone who had greater effectiveness than her own doctor in defining the nature of her problem and what should be done. By the time she encountered him, she was apprehensive lest she was not able to give a clear and precise account of her problems; she felt awkward, too, in confiding in a stranger, particularly those fantasies and fears that so disturbed her in the early hours of the morning. Dr J. greeted her in a polite, but busy and professional manner, getting quickly to the point of his many questions, which seemed both more numerous, organized and difficult to interrupt than those of her own doctor. Perhaps to her relief, he did not dwell on her emotional turbulence on waking, and passed quickly on to the questions concerning her physical symptoms. Mrs G. then underwent a number of physical investigations which, the doctor explained, would help him locate the source of her pain. Dr J. was, perhaps even more than Dr H., invested in doing this with speed and finality; he had spent many arduous years learning the required skills, and his professional status depended on his being seen to exercise them. He may have been a little dismayed, then, that Mrs G.'s physical examination, radiography and cardiograph were unremarkable, as he now had less definitive material with which to make his decision. 'I think your pains are caused by mild angina which isn't yet serious, and so isn't reflected in any of the tests', he explained to her, before elaborating the physical meaning of this, and the treatment he was prescribing for her. Mrs G.'s complaint was not typical of the diagnosis he made, but her answers to his questions suggested it as a real possibility, and Dr J. thought it was too important a diagnosis to be missed. He 'discharged Mrs G. back to her doctor', therefore, thinking he had defined the nature of her complaint and initiated a 'policy of management'. As before, let us distance ourselves a little more from this situation and look at the emergent patterns. Mrs G.'s mosaic of physical sensations, thoughts and feelings has been sampled by Dr J., who has reorganized and redefined them according to his own method of perception (the physical examination) and conception (his deductive process of making a medical diagnosis). His own feelings while doing this were not within his awareness, partly because they did not fit into this way of 'diagnosing' a patient's problems. Mrs G. came to the doctor with `dis-ease' which she expressed in her own language, but could find no personal meaning for; she leaves him with `disease' which is now expressed in the doctor's language, and to which he confers a meaning, which he must explain to her. Her own framework of experience with regard to her symptoms has become engulfed by the doctor’s concept. A consequence of her suffering from 'disease' rather than `dis-ease' is that she can do little about it, except obey the doctor's instructions. It is as if her dis-ease, which has become transformed into disease, is now the doctor's property, though unfortunately residing in her body; he knows about it, defines it in his language, `treats' or 'manages' or 'cures' the affliction, which she accommodates as an involuntary host. This process of 'didacticism' is illustrated in Figure 3.
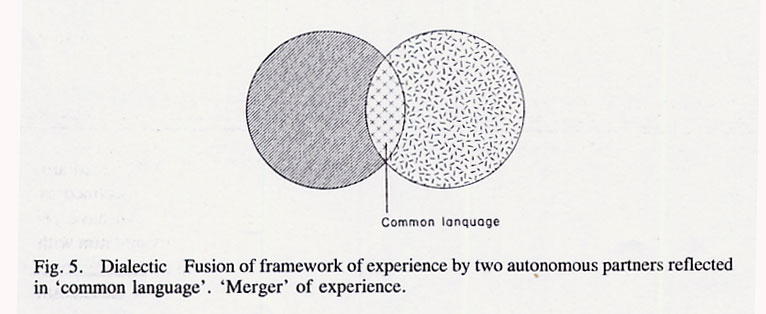
Note that the 'Free-Trade' profile of the dialogue has changed into a 'take over', where one has 'engulfed' the other; the interchange now is not 'free', but organized and structured by one (the doctor), while the other (the patient), becomes a passive recipient. In the illustration, the patient is shown as being largely encompassed, which is true in a psychological and social sense as long as they are together, and is one of the most important features of this didactic approach. The patient here is protected and carried much as a kangaroo in its mother's pouch and, as in this analogy, it necessarily involves an abdication of autonomy, self-definition and self-determination on the part of one of the parties, while the other takes on these functions for the two of them. Didacticism is thus part of the way 'regression' and 'dependency' become organized professionally. Whether or not this is welcome, or ultimately advantageous to one, or other, or both parties is a complex issue which will be explored later. Clearly, if Mrs G., for example, was overcome with acute and severe chest pains and breathlessness, she would almost certainly welcome the opportunity to abdicate all responsibility for understanding or reacting to her experience while critically ill. On the other hand, the excessive or ill-timed use of didacticism will lead to unwarranted intrusion and control, with its later sequels of passivity, resentment and 'guerrilla warfare' of the psychological kind. In Figure 3, which may illustrate Mrs G. and Dr J., Mrs G. is not totally encompassed, retains her own boundary and a space between the two. She still knows who she is, and can 'squeeze her way out' of this didactic arrangement if she so chooses. This is not so in extreme forms of didacticism. Within the healthcare field this would be illustrated by the critically ill patient in an intensive care unit who is physically encompassed by technology, or the institutionalized mentally ill who are contained and surrounded by a hospital environment. Such a situation is shown in Figure 4, and the analogy here could be made with the baby in utero; protection enclosure and dependence are complete — there is little possibility here for the self's assertion or expression.
Dialectic: the intimate encounter Situation 3: Mrs G. was at first comforted and reassured by Dr J.'s authoritative and knowledgeable manner and the many tests he performed to see what was wrong with her. Unfortunately, the tablets he gave her didn't seem to make any difference to her symptoms, and her own doctor at first responded by increasing the dose, again without effect. The next time she saw Dr H., he seemed less busy than usual, and Mrs G. felt under less pressure to produce a rapid précis of her experience, so as 'not to waste the doctor's time'. Dr H., partly due to the reduced demands on him, felt fresher and more receptive than he had been. when Mrs G. had previously seen him and, as she walked into his consulting room, he paid attention to a sudden feeling of sadness arising in him, a tugging sensation located in his chest, as if she had brought the feeling in with her. In the wake of this clear but unexpected visceral signal, he recalled the death of her husband, Harry, six months previously — an event which he had heard about indirectly, and which, for some reason, had previously eluded his focus. When she went on to talk of her thoracic discomfort, he asked her to elaborate it in her own words: 'it's like a knot here’ (rubbing the front of her left chest), ‘as if there's something there that's going to burst, and then I go dizzy and feel I can't breathe . . .’. Dr G. then asked: `When you lie awake at night, what do you think about?' Mrs G.'s eyes moistened briefly, as she quickly looked up into the corner of the room, simultaneously biting her lower lip: `Oh, I don't know . . . silly things, you know. It's difficult to say . . .’ Although not finishing her sentence, she looked at Dr G. deliberately and directly, a desolate but tacit gaze. Dr H. paused a couple of seconds, sat forward a little closer to her, saying gently and tentatively: `As you're talking, I have the sense that you feel sadder and more full of grief than you've conveyed to anyone . . . I'm wondering, too, about how much you want to say to Harry, about his leaving you, about being left on your own'. Mrs G. now sat forward, allowing herself to lean on the doctor's desk and saying: `Oh yes . . . you seem to understand that. There's so much of it inside of me, pulling my mind in different directions; but I've always been one to keep a brave face . . . my daughters tell me I've been “wonderful” the way I've coped, and I haven't wanted to tell them just how bad I've felt, how lonely I feel . . .’, she shrugged, as if discounting the interest of this to anyone but herself. Dr H. offered an image that surfaced and crystallised in his awareness: `It's like you've had to deal, very much on your own, with two broken hearts; the one that killed Harry and the one that you're left alive with, that hurts when you're most alone in the middle of the night.' `I don't know which I am; full of pain, hurting because I'm still alive when he's gone, or whether I'm just dead somehow, like Harry on the inside, although on the outside I'm just the same . . . can you understand that?' `Yes, the broken heart that gave up, and the one that has to carry on painfully — it's like you have them both inside of you . . . it takes a long time for that kind of pain and emptiness to go away; to have your heart touched or warmed, so that you know you're alive, and you know you want to be alive. There are times when we have to die a bit first… to come alive again'. `I think I've known that, at times, anyway, but it feels so much better just hearing you say it. It makes it more real somehow . . . like I know where I am and what I'm going through'. Mrs G. looked at the doctor sadly, but with less desolation than before; as if her heart was enlivened just a little already. The two of them sat together quietly for half a minute in a silence that was consummate and autumnal, as if they both needed a little time to digest, each in the company of the other, what they had produced together. Mrs G., slowly straightening herself from the doctor's desk that she had been leaning against, gathered her coat and bag together, saying thoughtfully: `I think I'll be alright, but it's hard. It's good to know you're here. Shall I come and see you next week, doctor?' `Yes, I think you need to, and I shall want to know how you are', replied Dr H., aware of a glowing sensation in his chest. Perhaps his heart, too, so often numbed by business and his didactic functions, was beginning to warm. Mrs G. did return regularly for some months, but on a very different basis from before. Her chest pains became far less alarming for her and eventually disappeared without any further medical initiative from Dr H. She seemed to seek him out as a companion, helping her through a difficult passage; she knew that he could not take away her dis-ease, but he could help understand it, bear it and perhaps resolve it. The doctor understood that his 'heart to heart' with his patient had eased the aching in her heart in a metaphorical and emotional sense; had this been reflected at a cellular level too? Dr H. wondered. Was she now perfusing her heart when before she was, literally physically, blocking it off? In any case, the doctor mused, their encounter seemed to have penetrated beyond the reach of his medication. The process and outcome of this last situation are clearly very different from the other two. Dr H. did not here attempt to quickly subsume his patient's account of her experience to his own prior concepts, but allowed himself a period of uncertainty, where various notions and possibilities were invented in the moment and could be offered to Mrs G. to sample, 'play with', explore, develop or discard as she wished. In doing this, the doctor paid equal attention to all the fragments of percept, affect and concept arising in both he and his patient; his own 'heaviness of heart' when she walked in the room was seen not as a contaminating influence to the medical interview, but as a potentially valuable emanation or expression which could be explored to find some kind of shared meaning. Likewise her involuntary physical reactions to his asking about her troublesome thoughts: when she turned her moistening eyes to the ceiling and bit her lip, Dr H. had a new if tentative understanding of her — 'In her mind's eye she continually sees Harry; the sadness she experiences is beyond her capacity to tell the living. She searches for him with her eyes but bites her lip to stop herself speaking of this', Dr H. had thought to himself, but also realized it was a subjective hypothesis to be offered to her to see if she would make sense of it. Mrs G. not only made sense of Dr H.'s metaphor of the 'broken heart', she elaborated on it, thus helping to create between the two of them a new and unique system of understanding, with its own symbols, metaphors and use of language. The physical movement of each toward the other physically, enacted what was happening at the psychological level; there was a convergence, even fusion, of their two worlds, so that the doctor's technical observations (P), his ideas about grief, body language, heart disease, ego-defence mechanisms and so forth (C), and the feelings arising in him (A), could be combined with the patient's disturbed bodily experiences and visual fantasies of her dead husband (P), her feelings of sadness and fear (A), and the notions she had about her physical disturbance and the life-passage she found herself in (C). The understanding that is constructed is new and unique and could only have arisen afresh in this situation; it could not have been organized or prescribed as a 'treatment'.
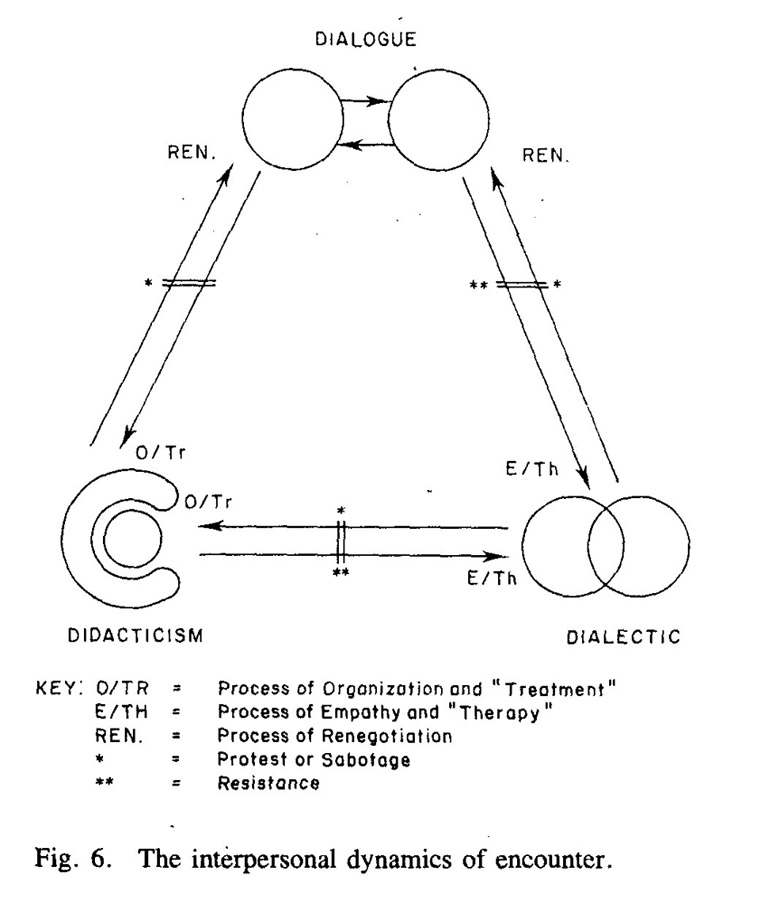
Figure 5 illustrates this process of 'dialectic', where a 'common language' is created in the area of fusion of two individual selves and world experiences. This common language is made up of the two individuals, but transcends them both in creating something new. In many ways it is equivalent to sexual union where fusion and interpenetration leads to new life which is made up of, but transcends, the two participants. Using the economic metaphor again, dialectic is akin to a 'merger'. It is similar, too, to the psychoanalyst Winnicott's1 notions of 'playing' and 'intimacy' where these are considered as the creation and elaboration of a 'transitional zone' — a fertile area of interchange and improvisation between the self and the other. The fact that this dialectical approach involves a certain mutuality or intimacy, implies certain conditions, restrictions and prerequisites; it is only possible and only a value, for example, where both partners are prepared to abandon their own frame of reference and integrate it into something as yet unknown. It also implies a giving up of the `control dimension' of the relationship, so that neither controls the other with regard to defining reality, using language, structuring the interchange, or prescribing what should be done. Clearly the didactic approach occupies the opposite pole from dialectic in these considerations. This intimacy, necessary for, and generated by, dialectic is crucial to certain phases and aspects of healing. In situation 3, Mrs G. had the sense of both understanding and being understood in a way that involved her own creativity and participation in the construction of the common language she achieved with her doctor. This being so, she felt empowered, dignified and compassionately accompanied in the experience, and enhanced in her capacity to clarify and express more. It is a fundamental psychodynamic principle that conflicts and dilemmas that remain unexpressed, unclear and unshared with others become amplified inside us and likely to become manifest in symptomatic difficulties. The act of understanding and entrusting our difficulties with another is often the first step in mastery and resolution. An important distinction should be made here between didactic and dialectic forms of insight and understanding. If Dr H. had prematurely said to her: `Part of your problem is that you have a masked depression. Your chest pain is due to you not letting go of Harry', he may have been correct and have been saying something similar, in content, to what he and Mrs G. had arrived at in situation 3. However, this didactic insight would have been inflicted on her, and would be far less likely to be helpful; the essential processes of trust, rapport, mutuality and common language are missing, and Mrs G. becomes, as she was in situation 2 with Dr J., the passive recipient of the doctor's organizing concepts. The art of integrating science Perhaps, though, Mrs G. needed to pass through a phase where she abdicated any knowledge of, or responsibility for, her symptoms and be cared for and defined by an authority figure, as she was by Dr J. In such a situation she may not have yet had the internal resources, or known Dr H. well enough, to have entrusted him with the faltering first steps involved in self-exploration and intimate disclosure. In short, she may have needed `treatment' by Dr J.'s organizing scientific concepts — didacticism — as a necessary phase or 'regression' where she felt protected, unchallenged and unalone. Only later, with the passage of time and the development of dialogue with Dr H., could she go on to take some responsibility for, and see some meaning in, her symptoms. The shared development by which this happened — dialectic — passed from a 'treatment' to a `therapy' situation, where the doctor was more responsive to, but less responsible for, Mrs G. The framework of understanding, and the language used to achieve this, changed from the doctor's scientific ideology to an `existential' mode, jointly formulated. Figure 6 illustrates the shifts involved in the three different kinds of encounter and the processes by which they occur.
Scientific medicine, as traditionally conceived and practised, involves a transmutation by the doctor of the dialogue he has with the patient, so that the patient submits to the treatment and abdicates responsibility for his distress. If either partner does not wish to continue this, or the treatment does not work, then, if the two wish to go on together, there must be a renegotiation through dialogue. If both are willing, able and motivated to find a more personal understanding and language for the problem, then there is a shift to a dialectic via the development of empathy. The naming of this change as 'therapy' (as opposed to 'treatment') implies the increased responsibility and activity of the patient. This can be abandoned by either renegotiation to dialogue, or reversion back to the treatment situation. Where one of the partners wishes to change the form of the encounter unilaterally, without some readiness on the part of the other, then certain defensive or sabotaging strategies will be used by the one pressurized to change. For example, the doctor who makes a premature shift into didacticism by diagnosing, say, premenstrual tension, is unlikely to get the patient to take the medication as prescribed. Another common example of this is the patient labelled 'schizophrenic' who will not adhere to drug regimes. The psychiatrist might say — didactically — that the patient's noncompliance is part of his 'schizophrenic illness', but it may instead reflect the psychiatrist's personality and training whereby he is resistant to, or incapable of, meeting his patient in a dialogue or dialectic. While 'protest' and 'sabotage' occur at largely conscious levels, 'resistance' operates unconsciously to defend a person against the authenticity, closeness and self-responsibility that ensue in any shift toward the intimacy of dialectic. Psychoanalytically, this term has traditionally been applied (didactically!) to patients, but it often works the other way round. Most hazardously in psychiatry, there is frequently a rapid moulding of a patient's communications so that they will fit into the doctor's diagnostic and treatment schemes; those that cannot be so tailored are either simply not heard or seen, or dismissed as lacking in 'clinical significance'. The fact that the doctor's didactic pronouncements and plans are often not effective may not lead him to renegotiating a dialogue, or attempting to construct a common language with his patient. In his own, and his profession's form of resistance, he may fall back even further into his didactic position by, for example, elaborating theories of 'psychopathology' of the patient’s condition — an attitude and endeavour which may be institutionalized and applauded by his colleagues but, paradoxically, lead to increasing alienation from his patients. Such a doctor's investment in maintaining a didactic position is often based on a fear of the reverse; that he himself becomes the one that is dependent, turbulent, powerless or vulnerable. Didacticism, at least while it operates, seems to confer immunity against such perils; the illusions, mechanisms and trappings of this have been dealt with in a previous article.2 Even if the doctor is not resistant to shifting away from his didactic position, many of his patients will be. The investment in another person for certainty, the power of transformation, warding off dangers of the unknown in ourselves and the world around us may be an illusion, but a comforting one. Authoritarian relationships and institutions often provide, too, a certain security and familiarity. Freedom and autonomy are often too much of a challenge and a burden.3 Thus, a doctor's attempt to provoke an unwilling patient to move away from their passive and defined role in the didactic arrangement will be met by some kind of sabotage or resistance. I remember a woman doctor who had been `treating', in an impotent and ritualistic form, a man for an endless stream of minor functional disorders, the favourite of which were 'sick headaches', for 15 years. He appeared, to the doctor, a stable, dull man whose lack of curiosity about the nature or meaning of his symptoms seemed part of his general passivity. One morning he came yet again, perhaps for the hundredth time, complaining in his stereotyped way of his inexorable complaints, asking: `Isn't there something else you can give me doctor?' `I wonder if there's something you ought to be giving yourself?', replied the doctor, for the first time attempting to break the pattern, she thought rather succinctly and profoundly. He looked askance at her: `Have you been on one of your new courses, doctor?', came the caustic retort, sly and rhetorical. She got the message, and he left with another prescription. In this situation the patient clearly wished his doctor to assume a didactic role and `treat' a `disease'; he resisted any attempt she might make to destructure their familiar roles, so that he might become more self-governing, self-responsible or self-aware by exploring the basis of his dis-ease. He wanted to be a patient. It can be seen here how the doctor wished to redefine the problem existentially, while the patient wished to continue with an organic or deterministic approach to his problem. Here lies a central ideological distinction between the dialectic and didactic approach. Didacticism tends to scientific determinism and the notion of mechanical disease, which can only be cured by the expert. Dialectic is an activity arising from an existential outlook, with an emphasis on pursuing personal responsibility and creating personal meaning. Psychotherapy, an area whose psychological and social politics is quite as difficult as conventional medicine, has practitioners whose method is often dominated by one of these modes. The orthodox psychoanalyst, for example, works on the assumption that the patient's 'psychopathology' depends on unconscious processes that only a trained psychoanalyst can understand and treat; Freud himself talked of patients 'submitting' to analysis. Existential psychotherapists, in contrast, emphasize mutuality, authenticity, intimacy and the attainment of common language as being therapeutic; there is here no prescribed treatment or organizing technical language. Clearly, in medicine, psychiatry, psychotherapy and all other forms of healing, we need to be able to shift with great dexterity between all three approaches with those that came to us. The skills of negotiating in dialogue, taking responsibility didactically, declining responsibility but allowing a new responsiveness in dialectic, are all cornerstones in the rich pattern of human intercourse that make up the healing arts. As in most other forms of intercourse, the problems arise when we are out of touch with one another’s internal worlds, or wanting to interact in the external world in different ways. For the healer rigorously trained in the didactic sciences, it often requires a significant change and development of personality to foster equal skill in the artistic exercise of dialectic. The perennial and rather simplistic question: ‘Is Medicine an Art or a Science?’ can be reformulated more precisely and meaningfully by asking instead: ‘How can we, with art and empathy, apply our medical science, and what is the science of applying this art and empathy?’. It is hoped that this description of the three types of encounter provides some basis for an answer. References 1. Winnicot, D.W. Playing and Reality. London, Tavistock Pubs., 1971. 2. Zigmond, D. ‘Physician Heal Thyself: The Paradox of Wounded Healer’. British Journal of Holistic Medicine, December 1984. Vol 1: 63-71. 3. Fromm, E. Escape from Freedom. New York, Holt, Rinehort and Winston, 1941. Holistic Medicine, Vol 2, 69-81 (1987)
Interested? Many articles exploring similar themes are available via David Zigmond’s home page on www.marco-learningsystems.com David Zigmond would be pleased to receive your FEEDBACK
|
||||||||